Biomechanical Consequences of a Tear of the Posterior Root of the Medial Meniscus
Similar to Total Meniscectomy
By Robert Allaire, MD, MuturiMuriuki, PhD, Lars Gilbertson, MD, and Christopher D. Harner, MD
Background: Tears of the posterior root of the medial meniscus are becoming increasingly recognized. They can cause
rapidly progressive arthritis, yet their biomechanical effects are not understood. The goal of this study was to determine the
effects of posterior root tears of the medialmeniscus and their repairs on tibiofemoral joint contact pressure and kinematics.
Methods:Nine fresh-frozen cadaver knees were used. An axial load of 1000 N was applied with a custom testing jig at
each of four knee-flexion angles: 0°, 30°, 60°, and 90°. The knees were otherwise unconstrained. Four conditions were
tested: (1) intact, (2) a posterior root tear of the medial meniscus, (3) a repaired posterior root tear, and (4) a total medial
meniscectomy. Fuji pressure-sensitive film was used to record the contact pressure and area for each testing condition.
Kinematic data were obtained by using a robotic arm to record the position of the knees for each loading condition. Threedimensional
knee kinematics were analyzed with customprograms with use of previously described transformations. The
measured variables were axial rotation, varus angulation, lateral translation, and anterior translation.
Results: In the medial compartment, a posterior root tear of the medial meniscus caused a 25% increase in peak contact
pressure compared with that found in the intact condition (p < 0.001). Repair restored the peak contact pressure to normal.
No difference was detected between the peak contact pressure after the totalmedialmeniscectomy and that associated with
the root tear. The peak contact pressure in the lateral compartment after the total medial meniscectomy was up to 13%
greater than that for all other conditions (p = 0.026). Significant increases in external rotation and lateral tibial translation,
compared with the values in the intact knee, were observed in association with the posterior root tear (2.98° and 0.84 mm,
respectively) and the meniscectomy (4.45° and 0.80 mm, respectively), and these increases were corrected by the repair.
Conclusions: This study demonstrated significant changes in contact pressure and knee joint kinematics due to a posterior
root tear of the medial meniscus. Root repair was successful in restoring joint biomechanics to within normal conditions.
Clinical Relevance: This study provides a biomechanical rationale for surgical repair of posterior root tears of the medial
meniscus. Clinical studies are required to define the appropriate patient population for, and to determine the clinical
efficacy of, surgical treatment of this injury.
In 1991, a tear of the posterior root of the medial meniscus
was first described in a twenty-year-old football player, in
whom arthroscopically confirmed degeneration of the articular
cartilage rapidly developed1. Since that time, posterior
root tears of the medial meniscus have become increasingly recognized
as other investigators have reported a similar, rapidly
progressive course of arthritis in their patients with this injury2-4.
Despite this troubling clinical course, little has been reported
regarding this injury in the orthopaedic literature.
In the musculoskeletal radiographic literature, there is a
growing body of evidence suggesting that a posterior root tear
of the medial meniscus leads to meniscal extrusion and is a
precursor to the development of degenerative knee arthritis4-9.
According to our current understanding of meniscal function,
a complete posterior root tear of the medial meniscus would
theoretically result in a functional meniscectomy in that complete
disruption of the circumferential fibers of the meniscus
prohibits the generation of hoop stress, which is crucial to me-
niscal function. Without a functional meniscus, the articular
cartilage of the knee is exposed to pathologic loads and subsequently
degenerates6,10-16. Despite these theoretical consequences,
we are not aware of any studies of the biomechanical consequences
of a tear of the posterior root of the medial meniscus.
The objective of this study was to describe the biomechanical
changes that occur with a posterior root tear of the
medial meniscus. Specifically, we had two aims: (1) to determine
the effects of a posterior root tear of the medial meniscus
and a total medial meniscectomy on tibiofemoral joint contact
stresses and kinematics in an in vitro model, and (2) to evaluate
the ability of a repair of the meniscal root tear to restore
joint contact stresses and kinematics. We hypothesized that a
posterior root tear of the medial meniscus would cause a significant
increase in joint contact pressure in the medial and
lateral compartments of the knee as well as an alteration in
joint kinematics, that the magnitude of this effect would be
similar to that caused by a total medial meniscectomy, and that
a repair of a posterior root tear of the medial meniscus would
restore joint contact pressure and kinematics to normal.
Materials and Methods
Specimens and Preparation
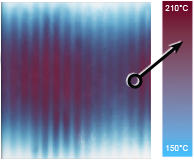
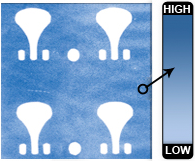
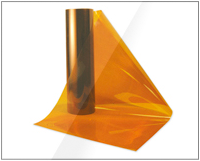
Nine fresh-frozen cadaver knees (five right and four left) from six male and three female donors ranging in age from twenty-four to fifty-four years at the time of death were radiographed to exclude the possibility of degenerative joint disease or other osseous abnormalities. The number of specimens was determined by performing a power analysis on the initial three specimens, with the assumption of a power of 80% and an alpha of 0.05. The analysis revealed that a sample size of six was required to demonstrate significance. Specimens were stored at 220°C, thawed at room temperature for twenty-four hours prior to dissection, and then examined to exclude the possibility of joint contracture, ligamentous or meniscal injuries, or indicators of degenerative joint disease. A minimally invasive technique preserving the integrity of all vital structures of the knee (Fig. 1, A and B) was used to gain access to the knee for pressure measurements with Fuji Prescale film (Fujifilm USA, Valhalla, New York). To gain access to the posterior aspect of the knee, all skin and subcutaneous tissues as well as the hamstrings and gastrocnemius were dissected while the distal tendinous insertions of the semimembranosus and biceps femoris were preserved. The knee joint and capsule remained intact except for a small (<1-cm) arthrotomy incision made posteromedially, inferior to the meniscus between the oblique popliteal ligament and the root of the medial meniscus. Care was taken not to damage the meniscus, the posterior cruciate ligament, the oblique popliteal ligament, or the root of the medial meniscus. Posterolaterally, a similar (<1-cm) submeniscal arthrotomy incision was made between the popliteus muscle and the root of the lateral meniscus with care taken to preserve both structures as well as the posterior cruciate ligament.


Testing Protocol
The femur and tibia were potted in epoxy compound and mounted in a custom testing jig that allowed positioning of the knee in 0°, 30°, 60°, and 90° of flexion without otherwise constraining the knee (Fig. 1, C). The flexion angles were tested sequentially, and were determined by the jig and confirmed with a MicroScribe 3DX digitizing robotic arm (Immersion, San Jose, California). The jig was mounted in a materials testing machine (TTS-25 kN; Adelaide Testing Machines, Toronto, Ontario, Canada), and each knee was loaded to 1000 Nof compression, which is consistent with the amount of compression used in previous studies of the human meniscus 17-24. No additional forces or moments were applied to the knee, and no attempt was made to place the knee in any specific position except for the described flexion angle. Thus, the position tested was the passive position dictated by the knee flexion angle, the inherent anatomy, and the applied load. Four meniscal conditions were tested: intact, a posterior root tear of the medial meniscus, a repaired posterior root tear of the medial meniscus, and a total medial meniscectomy. According to the senior author's (C.D.H.) technique, the posterior root tear of the medial meniscus was repaired in an open manner with two number-2 Ticron horizontal mattress sutures (Davis and Geck,Wayne, New Jersey) through the meniscal root. The free ends were tied over a button after they were passed through a bone tunnel that had been drilled from the anterolateral aspect of the tibia to the root insertion site with use of an Arthrex anterior cruciate ligament tunnel guide (Arthrex, Naples, Florida) (Fig. 2). A total medial meniscectomy was performed by removing the entire medial meniscus but preserving the medial collateral ligament and the coronary ligaments.
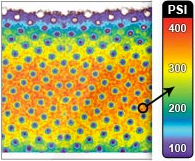
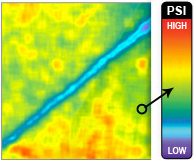
Prior to each application of load, a Fuji film packet was inserted through the anterior arthrotomies both medially and laterally under the meniscus. Once load was applied, a blunt wire was inserted through each of the previously drilled tunnels to mark the position of the film relative to the articular surface of the tibia. Load was applied for two minutes to comply with the manufacturer's recommendations and in agreement with our calibration protocol to allow accurate quantification of the pressures. For each loading condition, two packets of super-low-pressure and two packets of low-pressure Fuji film were used, resulting in a total of four trials for each meniscal condition and flexion angle.

Two-factor repeated-measures analysis of variance with a significance level of p < 0.05 was used to detect the overall effect, pooled across all flexion angles, of the meniscal condition on contact pressure, contact area, and kinematics. This also allowed analysis of any interaction between the variables. Single-factor repeated-measures analysis of variance with a significance level of p < 0.05 was used to detect the effects of eachmeniscal condition at the specific flexion angles. Least-significant-difference posthoc analysis was used.
Results
Contact Pressure and Area
When pooled across all flexion angles, the overall peak
contact pressure in the medial compartment was significantly
increased by a posterior root tear of themedialmeniscus as
compared with the pressure in the intact knee (125.4%, p <
0.001, Fig. 3). Repair of the posterior root tear of the medial
meniscus restored the overall peak contact pressure to control
values. No difference was detected between the effects of the
posterior root tear of the medial meniscus and the total medial
meniscectomy on the overall peak contact pressure in the medial
compartment. In the lateral compartment, no differences
were detected among the intact, root-tear, and root-repair conditions,
but the peak contact pressures for these conditions were
all significantly less than that after the total medial meniscectomy
(p = 0.029, p = 0.023, and p = 0.001 compared with the
intact, root-tear, and root-repair conditions, respectively). The
joint contact area decreased in the medial compartment as the
peak contact pressure increased (Fig. 3). The meniscectomy had
the largest effect on the joint contact area. Two-factor repeatedmeasures
analysis of variance revealed no significant interactions
between variables.
No significant effects on the peak contact pressures in
the medial compartment were noted at 0° of knee flexion (Fig.
4). At 30°, 60°, and 90° of knee flexion, the results were similar
to the overall results reported above. A posterior root tear of
the medial meniscus caused a significant increase in the peak
medial compartment pressure when compared with the pressure
in the intact condition (p < 0.001 at 30°, 60°, and 90°).
The root repair restored the peak contact pressure to that in the
intact knee. No differences were detected between the pressure
in the intact knee and that associated with the repair or between
the pressure associated with the root tear and that as-sociated with the total medial meniscectomy.
The contact area in the medial compartment showed similar reciprocal changes
throughout flexion, with the notable exception that, compared
with all other meniscal conditions, the totalmedialmeniscectomy
resulted in significantly lower contact areas at all flexion angles
(p < 0.05 for all flexion angles and comparisons; see Appendix).

Kinematics
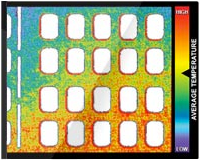
Three of the specimens could not be included in the kinematic analysis because technical malfunctions had resulted in uninterpretable data; this left six specimens available for this analysis (data summarized in the Appendix). When pooled across all flexion angles, external rotation was found to have increased in association with the posterior root tear of the medial meniscus while the root repair restored rotation to baseline values; the total medial meniscectomy further increased external rotation (Fig. 5). This effect was found to be significant when the root-tear condition was compared with the intact (p = 0.009) and root-repair (p = 0.003) conditions and when the total medial meniscectomy was compared with the root repair condition (p = 0.037). Lateral translation of the tibia relative to the femur increased in association with the root tear and was corrected by the root repair; the total medial meniscectomy also increased lateral translation. The difference in lateral translation was found to be significant when the roottear condition was compared with the root-repair condition (p = 0.011) as well as when the total medial meniscectomy was compared with the intact (p = 0.039) and root-repair (p = 0.003) conditions. There was a trend toward increased varus alignment in association with the root tear, which was corrected by the root repair; the total medial meniscectomy also increased varus alignment. This effect was found to be significant when the total medial meniscectomy was compared with the root-repair condition (p = 0.017). Anterior translation of the tibia relative to the femur also increased with injury to the root, with the difference reaching significance when the total medial meniscectomy and intact states were compared (p = 0.032). No significant difference in any kinematic measurement was found between the intact and root-repair conditions or between the root-tear and total medial meniscectomy conditions.

The posterior root tear of the medial meniscus increased lateral tibial translation, and the posterior medial meniscal root repair corrected it at all flexion angles; the total medial meniscectomy also increased lateral tibial translation (Fig. 7). This effect was found to be significant at 30° when the total medial meniscectomy was compared with the intact (p = 0.041) and root-repair (p = 0.040) conditions, at 60° when the root-tear condition was compared with the intact (p < 0.001) and rootrepair (p = 0.005) conditions as well as when the total medial meniscectomy was compared with the intact condition (p = 0.002), and at 90° when the root-repair condition was compared with root-tear (p = 0.049) and total medial meniscectomy (p = 0.001) conditions. No difference was detected between the intact and root-repair conditions or between the root-tear and total medial meniscectomy conditions at any knee position.
The overall trend toward increased varus angulation in association with the posterior root tear and correction by the root repair was observed at 0°, 30°, and 90° of flexion (see Appendix). The root tear caused a significant increase in varus alignment at 30° when compared with that associated with the intact (p = 0.035) and root-repair (p = 0.030) conditions. The root repair overcorrected the varus alignment at 90°. No difference in varus angulation was detected between the root-tear and total medial meniscectomy conditions at any flexion angle.

Discussion
This study demonstrated that a posterior root tear of the medial
meniscus causes increased knee contact pressures and kinematic
derangements in a cadaver model. The peak pressures in the
medial compartment were significantly elevated by a posterior
root tear of themedialmeniscus and were restored to baseline after
a repair of such a tear. Both a total medial meniscectomy and a
posterior root tear of the medial meniscus significantly altered
knee kinematics.
Because of the small number of specimens in our study,we
were unable to draw any definitive conclusions regarding the
biomechanical equivalence of a posterior root tear of the medial
meniscus and a total medial meniscectomy. (A power analysis
with the assumption of a power of 80% and a = 0.05 demonstrated
that 2977 specimens would be required to show a difference.)
However,we did not detect a difference in anymeasured
variable between the root-tear and total medial meniscectomy
conditions, a finding that is in agreement with our hypothesis
that loss of the function of the posterior root of the medial meniscus
results in a functional meniscectomy. Similarly, we were
unable to conclude that a repair of the posterior root of the
medial meniscus is equivalent to an intact meniscus. (One hundred
and forty-two specimenswould have been required to show
a difference, according to our power analysis.)However, we were
able to demonstrate a significant improvement in medial compartment
contact pressure, tibial external rotation, and lateral
tibial translation between the root-tear and root-repair conditions.
The negative effect of mechanical pressure on articular
cartilage has been well documented26-29. Surgical intervention to
restore a deficient posterior root of the medial meniscus may
restore normal knee biomechanics and prevent the development
of early degenerative joint disease in an appropriately
selected patient population.
Posterior root tears of the medial meniscus are an underrecognized
clinical entity that result in rapidly progressive degenerative
arthritis1,2,7,30. Since the original report by Pagnani
et al.1, little progress has been made in terms of treating or
understanding this injury. Lerer et al.7 evaluated patients with an
extrusion of the medial meniscus and found significant associations
between pathologic extrusion, loss of articular cartilage,
and a posterior root tear of the medial meniscus that resulted in
loss of meniscal function. These findings led the authors to
conclude that techniques for the repair of posterior root tears of
the medial meniscus should be developed to slow the progression
of, and perhaps prevent the development of, osteoarthritis.
Beasley et al.2 described a cohort of patients with a
posterior root tear of the medial meniscus who were distributed
bimodally into a middle-aged group with a body mass
index of >30 and a younger, athletic group who had sustained
an acute knee injury. None of these patients had a posterior
root repair, and they uniformly had rapidly progressive degenerative
knee disease. Ahn et al. described repair of posterior
root tears of the medial meniscus with a technique similar to
that used in our study3.We are not aware of any biomechanical
studies of posterior root tears of the medial meniscus.
Multiple studies have demonstrated increased contact
pressure and decreased contact area in the medial compartment
of knees that underwent a total medial meniscectomy15-17,21,24,31,32.
Our results are consistent with those reports. Many researchers
have studied the effects of partial meniscectomy and meniscal
transplant onmedial compartment contact pressure and area33-38.
The effect of clinically relevant tears on joint contact pressure
and area has not been as extensively studied16,17. Several authors
have evaluated bucket-handle tears of the medial meniscus but
not the effect of this tear or its repair on joint contact pressure
20,39,40. Ours is the only study of which we are aware to focus
on the effect of a posterior root tear of the medial meniscus
and its repair on knee contact pressure and kinematics.
This study helps to describe the role of the meniscus in
knee kinematics in multiple degrees of freedom. Similar to the
findings reported by previous authors41, we demonstrated increased
anterior tibial translation in association with medial
meniscectomy. This is thought to be secondary to a buttress effect
of the posterior horn of themedialmeniscus against the posterior
femoral condyle as the tibia is translated anteriorly. We additionally
demonstrated increased lateral tibial translation in association
with loss of the medial meniscus. By a similarmechanism,
the intact middle horn of the medial meniscus buttresses against
the medial portion of the medial femoral condyle. Loss of this
buttress allows the tibia to translate laterally relative to the femur.
The role of the medial meniscus in rotational knee kinematics
can be explained in a similar manner. Our data demonstrated
increased external tibial rotation of up to 6° with loss
of themedialmeniscus. The intact cruciate ligaments and lateral
compartment of the knee hold the central and lateral portions
of the knee relatively fixed so that when the medial aspect of the
tibia subluxates anteriorly it creates a rotational moment, thus
resulting in external rotation. The change in varus alignment
may be understood in a similar manner. Lateral translation in
combination with loss of a spacer on the medial side of the knee
allows compression of the medial compartment, resulting in
varus alignment.
These kinematic changes are likely responsible for the
changes in lateral compartment pressures demonstrated in this
study and in previous biomechanical investigations23,36,42. As the
tibia subluxates laterally, and externally rotates, the lateral tibial
spine is brought closer to the lateral femoral condyle, resulting
in pathologic loading of the articular cartilage and subsequent
degeneration. This corresponds with our clinical observations
that chondrosis develops over the lateral tibial spine in patients
who have a normal lateral meniscus in the presence of a posterior
root tear of the medial meniscus (see Appendix). We did
not observe any changes in lateral compartment contact area
despite significant changes in lateral peak contact pressure after
medialmeniscectomy.We did notmeasuremean pressure, which
would be expected to vary inversely with the contact area.
Our model was designed in an attempt to reproduce as
accurately as possible the in vivo situation, but, as is the case
with all in vitro studies, ours has several limitations. It is a
cadaver model in which we are unable to reproduce normal
tissue biology, including muscle contractions, proprioception,
and healing. We used a simple, static loading scheme without
applying any rotational or translational forces, and we did not
load any of the muscles around the knee, thus limiting our
ability to extrapolate these data to a clinical population. Furthermore,
the use of a passive loading scheme may have resulted
in underestimation or overestimation of both the kinematic and
the pressure effects.We did not use an arthroscopic technique to
performour repairs. Because of improved access to the posterior
root of the medial meniscus, our repairs may have been better
than those achievable arthroscopically. Some knee dissection
was necessary to obtain intra-articular pressure measurements.
Previous authors have disarticulated the knee, performed extensive
arthrotomies, and performed osteotomies to gain access
to the knee. Our approach preserved all of the described stabilizers
of the knee without disrupting the articular anatomy,
but the small knee arthrotomies and superficial dissection still
may have had an effect on the knee biomechanics.
In conclusion, as is the case for any cadaver study, extrapolation
to a clinical patient population should be done
cautiously. This study demonstrated the deleterious effects of a
posterior root tear of the medial meniscus on knee biomechanics
and showed this injury to be similar to a total medial
meniscectomy in terms of its effects on knee joint contact
pressure and kinematics. This study also suggests a biomechanical
Appendix
 A more detailed description of the methods used to analyze
joint contact area- and pressure and knee kinematics;
a table presenting kinematic data; and figures showing
medial compartment contact area, lateral compartment peak
contact pressure, varus angulation, anterior tibial translation,
and lateral compartment wear associated with the posterior
root tears of the medial meniscus are available with the electronic
versions of this article, on our web site at jbjs.org (go to
the article citation and click on ‘‘Supplementary Material'')
and on our quarterly CD/DVD (call our subscription department,
at 781-449-9780, to order the CD or DVD).
A more detailed description of the methods used to analyze
joint contact area- and pressure and knee kinematics;
a table presenting kinematic data; and figures showing
medial compartment contact area, lateral compartment peak
contact pressure, varus angulation, anterior tibial translation,
and lateral compartment wear associated with the posterior
root tears of the medial meniscus are available with the electronic
versions of this article, on our web site at jbjs.org (go to
the article citation and click on ‘‘Supplementary Material'')
and on our quarterly CD/DVD (call our subscription department,
at 781-449-9780, to order the CD or DVD).
Muturi Muriuki, PhD
Department of Orthopaedic Surgery, University of Pittsburgh,
3471 Fifth Avenue, Suite 1011, Pittsburgh, PA 15213. E-mail address
for R. Allaire: [email protected]
Lars Gilbertson, MD
Spine Institute Research Laboratory, Cleveland Clinic,
9500 Euclid Avenue, Cleveland, OH 44195
Christopher D. Harner, MD
Center for Sports Medicine, University of Pittsburgh
References
2. Beasley L, Armfield RD, West R, Irrgang J, Gilbert M, Harner CD. Medial meniscus root tears: an unsolved problem—demographic, radiographic, and arthroscopic findings. Pittsburgh Orthop J. 2005;16:155.
3. Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15:1510-3.
4. Jones AO, Houang MT, Low RS, Wood DG. Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol. 2006;50: 306-13.
5. Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage. 1999;7:526-32.
6. Kenny C. Radial displacement of the medial meniscus and Fairbank's signs. Clin Orthop Relat Res. 1997;339:163-73.
7. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33: 569-74.
8. Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54:502-6.
9. Sugita T, Kawamata T, Ohnuma M, Yoshizumi Y, Sato K. Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop Relat Res. 2001;387:171-7.
10. Fairbank T. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664-70.
11. Hede A, Larsen E, Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16:122-5.
12. Hede A, Larsen E, Sandberg H. Partial versus total meniscectomy. A prospective, randomised study with long-term follow-up. J Bone Joint Surg Br. 1992;74:118-21.
13. Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, Guermazi A, Grigorian M, Gale D, Felson DT. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795-801.
14. Jaureguito JW, Elliot JS, Lietner T, Dixon LB, Reider B. The effects of arthroscopic partial lateral meniscectomy in an otherwise normal knee: a retrospective review of functional, clinical, and radiographic results. Arthroscopy. 1995;11:29-36.
15. Krause WR, Pope MH, Johnson RJ, Wilder DG. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599-604.
16. Radin EL, de Lamotte F, Maquet P. Role of the menisci in the distribution of stress in the knee. Clin Orthop Relat Res. 1984;185:290-4.
17. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270-5.
18. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871-9.
19. Brown TD, Shaw DT. In vitro contact stress distribution on the femoral condyles. J Orthop Res. 1984;2:190-9.
20. Becker R, Wirz D, Wolf C, G¨opfert B, Nebelung W, Friederich N. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg. 2005;125:254-60.
21. Bourne RB, Finlay JB, Papadopoulos P, Andreae P. The effect of medial meniscectomy on strain distribution in the proximal part of the tibia. J Bone Joint Surg Am. 1984;66:1431-7.
22. Harris ML, Morberg P, Bruce WJ, Walsh WR. An improved method for measuring tibiofemoral contact areas in total knee arthroplasty: a comparison of K-scan sensor and Fuji film. J Biomech. 1999;32:951-8.
23. Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993; 17:214-8.
24. Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184-92.
25. Fischer KJ, Manson TT, Pfaeffle HJ, Tomaino MM, Woo SL. A method for measuring joint kinematics designed for accurate registration of kinematic data to models constructed from CT data. J Biomech. 2001;34:377-83.
26. Ewers BJ, Dvoracek-Driksna D, Orth MW, Haut RC. The extent of matrix damage and chondrocyte death in mechanically traumatized articular cartilage explants depends on rate of loading. J Orthop Res. 2001;19:779-84.
27. Loening AM, James IE, Levenston ME, Badger AM, Frank EH, Kurz B, Nuttall ME, Hung HH, Blake SM, Grodzinsky AJ, Lark MW. Injurious mechanical compression of bovine articular cartilage induces chondrocyte apoptosis. Arch Biochem Biophys. 2000;381:205-12.
28. Lucchinetti E, Adams CS, Horton WE Jr, Torzilli PA. Cartilage viability after repetitive loading: a preliminary report. Osteoarthritis Cartilage. 2002;10:71-81.
29. Quinn TM, Allen RG, Schalet BJ, Perumbuli P, Hunziker EB. Matrix and cell injury due to sub-impact loading of adult bovine articular cartilage explants: effects of strain rate and peak stress. J Orthop Res. 2001;19:242-9.
30. Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373-8.
31. Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;149:283-90.
32. McKinley TO, English DK, Bay BK. Trabecular bone strain changes resulting from partial and complete meniscectomy. Clin Orthop Relat Res. 2003;407: 259-67.
33. Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12: 174-81.
34. Huang A, Hull ML, Howell SM, Haut Donahue T. Identification of crosssectional parameters of lateral meniscal allografts that predict tibial contact pressure in human cadaveric knees. J Biomech Eng. 2002;124:481-9.
35. Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med. 1997;25:692-8.
36. Pe˜na E, Calvo B, Martı´nez MA, Palanca D, Doblar´e M. Finite element analysis of the effect of meniscal tears and meniscectomies on human knee biomechanics. Clin Biomech (Bristol, Avon). 2005;20:498-507.
37. Sekaran SV, Hull ML, Howell SM. Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med. 2002;30:74-82.
38. Zielinska B, Donahue TL. 3D finite element model of meniscectomy: changes in joint contact behavior. J Biomech Eng. 2006;128:115-23.
39. D¨urselen L, Schneider J, Galler M, Claes LE, Bauer G. Cyclic joint loading can affect the initial stability of meniscal fixation implants. Clin Biomech (Bristol, Avon). 2003;18:44-9.
40. Richards DP, Barber FA, Herbert MA. Compressive loads in longitudinal lateral meniscus tears: a biomechanical study in porcine knees. Arthroscopy. 2005;21:1452-6.
41. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anteriorposterior motion of the knee. J Bone Joint Surg Am. 1982;64:883-8.
42. Pe˜na E, Calvo B, Martinez MA, Palanca D, Doblar´e M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res. 2006;24:1001-10.
43. Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints—Part I: Tibial surface of the knee. J Biomech Eng. 1983;105: 216-25.
44. Brand RJ. Joint contact stress: a reasonable surrogate for biological processes? Iowa Orthop J. 2005;25:82-94.
45. Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med. 2001; 29:403-9.
46. McDermott ID, Sharifi F, Bull AM, Gupte CM, Thomas RW, Amis AA. An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc. 2004;12:130-5.
47. Hale JE, Brown TD. Contact stress gradient detection limits of Pressensor film. J Biomech Eng. 1992;114:352-7.
48. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136-44.